In a recent AcademyHealth post I wrote about polypharmacy, which is a risk factor for adverse drug events (ADEs).* But, ADEs constitute a larger issue with a substantial literature — there are many other contributors to them besides polypharmacy.
The 2014** National Action Plan for Adverse Drug Event Prevention is a useful guide. Of course there are many sources of hospital complications and adverse events, but it notes that ADEs comprise one-third of them, contributing to longer hospital stays to the tune of 1.7 to 4.6 days. One study found that ADEs account for two-thirds of post-discharge complications and that 24% of them are preventable.
One-third of inpatient stays are by adults 65 years old and older. However, 53% of those stays are accompanied by an ADE. Contrast that with "only" 30% for 45-64 year olds (see chart below).
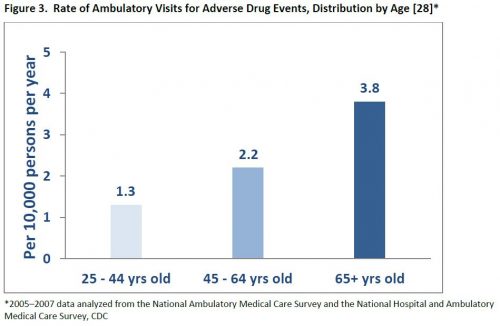
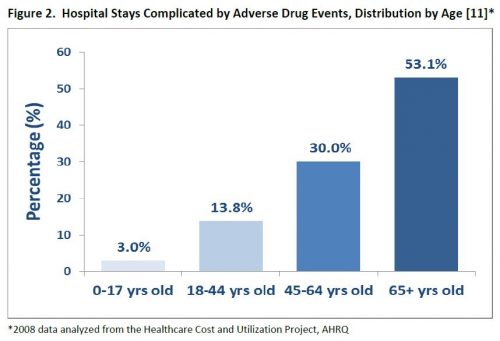 Likewise, older adults are more likely to see a physician visit the ED due to an ADE (see chart below). ADEs contribute to 3.5 million physician office visits, and 1 million ED visits annually.
Likewise, older adults are more likely to see a physician visit the ED due to an ADE (see chart below). ADEs contribute to 3.5 million physician office visits, and 1 million ED visits annually.
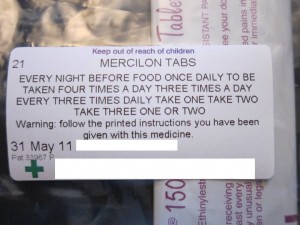
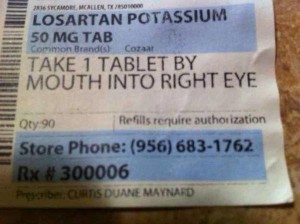
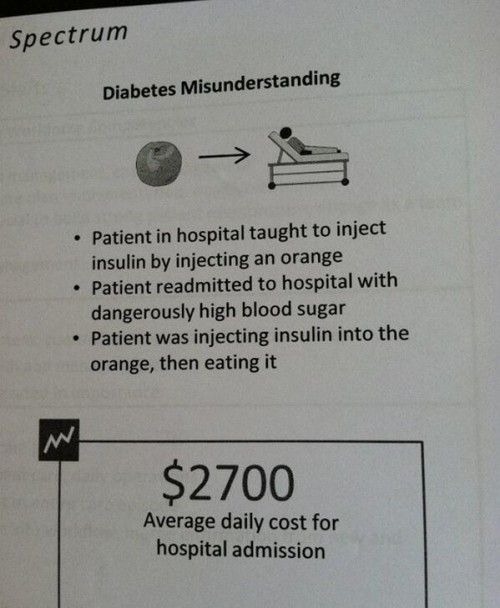
How do ADEs arise? There are lots of places for errors to enter the process. Once a drug is prescribed, that prescription needs to be communicated to the point of dispensing. It needs to be dispensed correctly. That requires the right labeling and, in some cases, compounding. Then the (correct) drug needs to administered to or by the (correct) patient at the right time, in the right manner, and with the right dose.
Studies document errors along this entire chain. Seven percent of inpatient drug orders are incorrectly prescribed. Eight percent of doses are administered incorrectly. For 70% of hospital admissions or discharges, providers don't properly take account of all the medications patients are on, which opens the door for adverse drug reactions and interactions. And many studies show that up to half the time, patients don't take drugs as prescribed, compromising care.
Newer technology — already implemented in many settings — can help. Electronic, rather than hand-written, prescriptions eliminate handwriting/reading errors. They permit automatic checks of conflicts and doses. They don't prevent all problems, but they solve more than they cause.
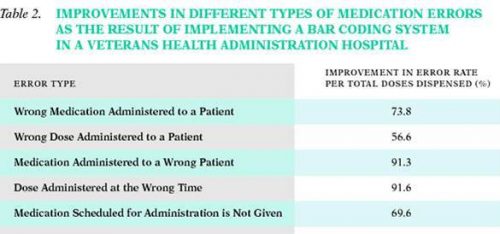
Bar coding in pharmacies and hospitals (of drugs, patients, and practitioners) all help get the right drugs to the right people at the right time and dose. For example, when one VA hospital implemented a bar coding system, error rates fell (chart below).
There's help for patients too. Text messaging and television ads can remind people to take their drugs as prescribed. To reduce medication errors, The Institute of Medicine recommends lower tech approaches.
One of the most effective ways to reduce medication errors is to move toward a model of health care where there is more of a partnership between patients and health care providers.
Indeed, patients often (though don't always) know when something isn't right, when they're feeling an unusual side effect, or when a prescription isn't consistent with their experience or what the doctor may have told them.
But, patients won't know when something is wrong or won't report it if patient-clinician communication is weak. This can lead to needless problems and expense.
Because ADEs can arise in many ways along the complex path from prescription to drug administration, many approaches are necessary to minimize them, including both high- and low-tech.
* An adverse drug event is any injury related to a drug used medically.
** As best I can tell, it was published in 2014, but there's no date on the publication itself, so I could be off by a year.