Though the Affordable Care Act (ACA) does not directly change the Veterans Health Administration (hereafter, VA), veterans are an important subgroup of those affected by the law. You might think coverage expansion is irrelevant to them because the VA provides care to veterans. Thought it's true that the VA does so, it's not the full story.
For one thing, the VA operates on a priority system. Veterans meeting the minimum duty requirements may apply for assignment into one of eight priority groups. The VA can, and has, suspended enrollment for lower priority groups, though no such suspensions are in place today. Additionally, cost sharing varies by priority group. Inpatient and outpatient VA care is free to low income veterans and those with the highest priority that have the most service-connected disabilities. Other VA enrollees are subject to copayments. VA-financed care can only be obtained at or arranged by VA facilities. Therefore, the distance a veteran lives from one is a barrier to access. Finally, waiting times can be longer than 25 days at 10% of VA facilities. This is, however, a shorter length of time than those that have been shown to lead to poorer outcomes.
Apart from all that, veterans are certainly eligible to enroll in other forms of coverage, like Medicaid, Medicare, and private plans. Most of them do, an indication that they value such coverage instead of or in addition to VA care. Since the ACA expands coverage options, it's of obvious relevance to veterans, as well as the VA, for which they may be substitutes. Moreover, some veterans remain uninsured, even counting the VA as a potential source of care.
In a presentation in November, as well as two Urban Institute publications (here and here), Jennifer Haley and Genevieve Kenney document uninsurance among veterans and the potential impact of the ACA. They estimated that 10.5% of nonelderly veterans are uninsured, which is lower than the nearly 18% of the general, nonelderly population (estimates as of 2010). More than one-third of these uninsured veterans report unmet health needs or delayed care due to cost.
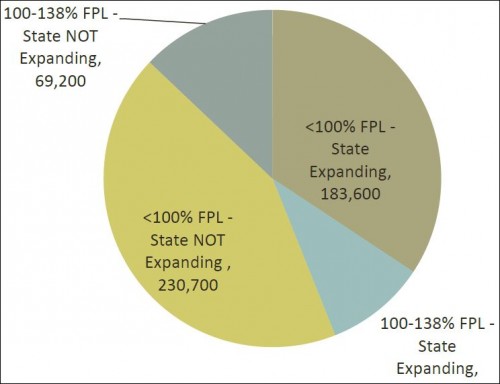
The Medicaid expansion could go a long way toward addressing these issues. The authors estimate that 4 in 10 uninsured veterans would qualify for Medicaid if it expanded in all states. However, most such veterans live in states that have, as of this writing, opted not to participate in the expansion.
Proportion of low-income veterans by state Medicaid expansion status [source]
Another 4 in 10 veterans have incomes below 400% of the federal poverty level (FPL), and so would qualify for subsidies toward purchase of exchange-based plans. This, combined with states' expansion of Medicaid -- albeit not universal -- would suggest that that fewer veterans might enroll for VA care or that the volume of VA use might decrease.
However, there are countervailing considerations. First, VA enrollment satisfies the individual mandate. This alone could encourage veterans to seek enrollment. Couple this with the lack of universal expansion of Medicaid, and it could lead to growing VA enrollment and use in some states. In addition, general awareness about the coverage requirement and availability of resources pertaining to coverage could increase interest in the VA as an option for veterans. Navigators and enrollment offices/programs could screen for veteran status to help identify those who are eligible for VA services.
It's not yet clear which set of forces will prevail. Will enrollment and utilization of VA care decline, due to the expansion of coverage options for veterans and all Americans (apart from low-income Americans in states not expanding Medicaid)? Or will VA enrollment and use increase due to the mandate and greater awareness of VA eligibility?
Though we don't know the answers today, we can be confident that with new coverage options, uninsurance and unmet need among veterans is going to fall, as it will for the non-veteran population.