Much has been made about the relationship between hospital readmission rates and mortality. Dead people can’t be readmitted, suggesting a negative correlation. On the other hand, decreases in both seem to be measures of quality, suggesting a positive correlation.
Harlan Krumholz and colleagues published a JAMA article last month that examines the correlation between risk-adjusted, 30-day readmission rates and mortality rates, both calculated on a fee-for-service Medicare cohort using CMS’s methodology. In particular, they examined patients discharged with a diagnosis of heart failure (HF), acute myocardial infarction (AMI), or pneumonia (PN). Correlations were not statistically significantly different from zero between mortality and readmission rates for the AMI and PN disease cohorts. For the HF cohort, the correlation point estimate was -0.17. Wanna see it?
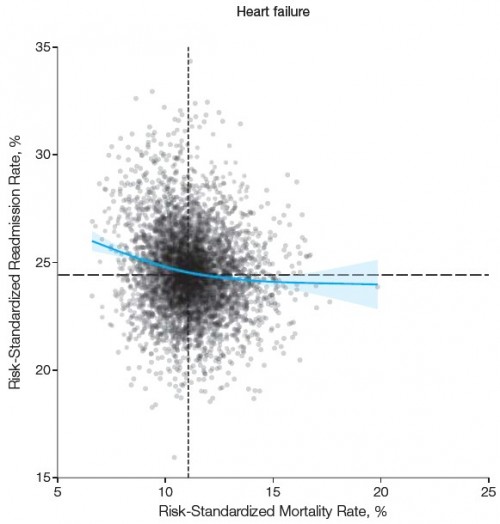 (Dashed lines are medians. The blue line is a cubic spline smooth regression. The shaded area designates the 95% confidence interval.)
The authors conclude that mortality and readmission rates measure different, nearly orthogonal aspects of quality.
(Dashed lines are medians. The blue line is a cubic spline smooth regression. The shaded area designates the 95% confidence interval.)
The authors conclude that mortality and readmission rates measure different, nearly orthogonal aspects of quality.
From a policy perspective, the independence of the measures is important. A strong inverse relationship might have implied that institutions would need to choose which measure to address. Our findings indicate that many institutions do well on mortality and readmission and that performance on one does not dictate performance on the other.Ashish Jha has another perspective. A quote doesn’t do justice to his argument, but here’s the key passage:
So if one measure of quality is external validity – being at least somewhat correlated with the gold standard (mortality rates) — how does the readmission measure do? In a paper published recently in JAMA, we see that readmission rates don’t do so well at all. Readmission rates are un-correlated with mortality rates. In fact, for one of the three conditions, the readmission rate seems to go the wrong way: the best hospitals for heart failure (i.e. those with the lowest mortality rates) have readmission rates that are actually higher. Not perfect. Readmissions seem to have little external validity as a quality measure. Readmissions are, however, correlated with two things: how sick your patients are, and how poor your patients are. We now have good data that the Hospital Readmission Reduction Program disproportionately penalizes big academic teaching hospitals (that care for the sickest patients) and safety-net hospitals (that care for the poorest).Ashish goes on to suggest readmission rates can still play a helpful role in motivating hospitals and health systems to improve. Maybe! I worry that they can also be gamed. Since they’re hardly correlated with mortality, we may not easily detect when they are. --Austin