As the accessibility of federal data continues to be threatened, another critically important data source has disappeared and may be permanently shut down. Despite being one of the most comprehensive, widely used sources of information about maternal and child health (MCH) in the United States, the future of the Pregnancy Risk Assessment Monitoring System (PRAMS) is in doubt. In March, the portal used by approved researchers to access PRAMS data was taken offline. The Centers for Disease Control and Prevention (CDC) website stated that the 2023 data would be available to states in March and that 2025 data collection would resume in April, but there is no indication that either action has been carried out (Figure 1). In fact, on April 1, as a part of the massive Department of Health and Human Services (HHS) layoffs, the entire PRAMS survey team at the CDC Department of Reproductive Health was laid off. Our analysis of publicly available spending data shows that yearly funding for PRAMS – which has been typically obligated to states in March – has not been obligated (Figure 2). The disappearance of existing data and grim uncertainty about the future of this survey have harmful implications for the health of mothers, infants, and families across the U.S., and it is critical that Health and Human Services Secretary Robert F. Kennedy, Jr. reverse this decision. However, states and localities have the opportunity to step in to continue the sustainability of PRAMS.
Figure 1: Screenshot of the CDC website from March 26, 2025 that says, “PRAMS 2023 data is anticipated to be available to sites by March 2025; PRAMS 2024 data collection is completed; and PRAMS 2025 birth cohort data collection is anticipated to begin by April 2025.”
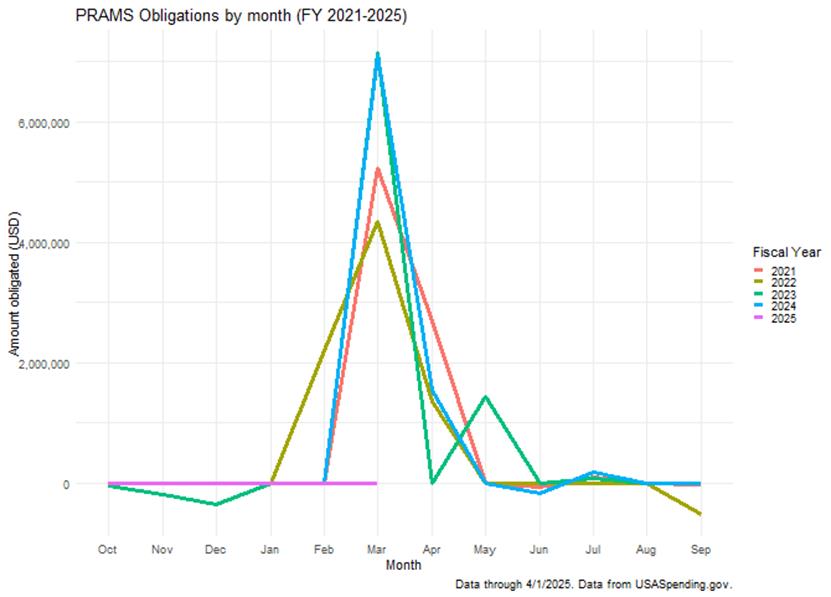
Figure 2:Chart that shows federal spending obligations to states for PRAMS in each month of fiscal years 2021-2025. In FY 2021-2024 the month with by far the greatest spending obligations is March; all other months have little to no spending obligations. There are no spending obligations in fiscal year 2025 as of April 1, 2025. Data are from USASpending.gov.
PRAMS is a survey about maternal health behaviors and experiences before, during, and after birth and asks questions about experiences of health care access, health behaviors, and socioeconomic factors such as insurance coverage and income. The survey data are linked to infant birth certificates, offering key insight into the ways that these maternal factors influence both maternal and infant health outcomes. Since 1998, PRAMS has been conducted through state-federal partnerships; forty-six states and four jurisdictions participated in 2024. States administer the survey while the CDC offers funding (approximately $175,000 annually per participating state), maintains a central data collection system, assists with survey design, and processes data. The data are then made publicly available each year and are used to inform and evaluate programs across the country that improve maternal and infant health.
Researchers, medical providers, and health departments have long relied on PRAMS data to identify key MCH issues, demonstrate the impact of MCH programming on families in their state, and advocate for continued funding for programs that work. For example, in West Virginia, PRAMS data were used to identify that state rates of smoking during pregnancy were much higher than the national average in 2018. Following this, MCH stakeholders in West Virginia began a large-scale effort to fund projects that would reduce the prevalence of smoking during pregnancy. One such program trained perinatal health care providers on how to screen patients for tobacco use and refer them to tobacco cessation programs. Another initiative integrated smoking cessation education into home visitations for pregnant individuals. With the implementation of this suite of programs, smoking during the last trimester of pregnancy dropped substantially – from 25 percent in 2018 to 10 percent in 2023.
Another example of how PRAMS has been used to identify critical MCH issues – and measure improvement – is in Pennsylvania. In 2015, MCH experts in the state identified an urgent need to reduce sudden infant death syndrome (SIDS) by increasing safe infant sleep practices. In addition to continuing and expanding programs like Cribs for Kids, which provided portable cribs and safety education to families, the state launched a multi-pronged messaging campaign to inform parents about safe sleep practices via social media, as well as brochures and posters in hospitals and on public transportation. PRAMS data has demonstrated that safe sleep practices have been on the rise in Pennsylvania since this issue was prioritized; between 2016 and 2022, the percent of mothers reporting placing their infant to sleep without soft objects or loose bedding rose from 46 percent to 65 percent.
The data provided by PRAMS has long been used to monitor MCH outcomes at the state and national level. Additionally, the centralized data collection system allows for easy comparison between states, so that we can learn what does and does not work to improve maternal health. Without access to this data, it will be near impossible to develop MCH programs that are responsive to changing state-level needs and priorities, or to monitor if existing programs are effectively improving MCH outcomes. This is particularly concerning with the maternal health crisis currently being faced by the U.S.
Given that the CDC may not continue to fulfill their long-standing obligation, state policymakers and researchers can step in to preserve this critical work. First, state legislatures can allocate necessary funding to sustain PRAMS. We’ve developed a policy brief template to help educate policymakers about PRAMS which can be customized for each state (access the customizable template here to download). Second, survey teams can develop their own data collection tools and infrastructure informed by existing, publicly available PRAMS protocol documents. Homegrown PRAMS surveys that do not rely on the CDC are already operating in cities like Pittsburgh and Philadelphia. States can learn from these self-sufficient city models. Finally, to maintain a key feature of PRAMS, cross-state comparability, MCH experts from across the U.S. could form a multi-state consortium which would work to standardize measures and promote cross-state learning. These steps can help states to preserve the continuity of PRAMS while its long-term fate remains uncertain at the federal level. As the only dataset to combine maternal health surveys capturing mothers’ experiences and behaviors with objective infant health outcomes data, it is imperative that PRAMS data continue to be collected and remain accessible.