In July, I wrote about a study by Christopher Afendulis, Michael Chernew, and Daniel Kessler that investigated the extent to which Medicare Advantage (MA) plans promoted better health outcomes relative to traditional, fee-for-service (FFS) Medicare. The work sheds light on whether MA's performance relative to FFS is entirely based on relatively healthier enrollees (favorable selection). The results suggested MA plans performed much better than FFS even apart from whatever favorable selection they receive, though one should be mindful of potential methodological issues yet to be addressed in the paper.
Subsequently, Health Affairs published a similarly themed study by John Ayanian and colleagues. Its focus relates to concerns with the incentives of MA payment methodology. Plans are paid a fixed, monthly, risk-adjusted rate per beneficiary to provide the Medicare benefit. This provides an incentive for plans to stint on care, pocketing whatever money is saved. No such incentive exists under FFS. Therefore, one might expect MA plans to perform worse -- or, at least, no better -- on process quality measures, relative to FFS plans. For, what would be the incentive to promote costly access that would enhance quality? (One incentive is that it reduces downstream costs. But it is very unlikely that better process quality is cost saving, and certainly not on the time scale that plans are likely to consider.)
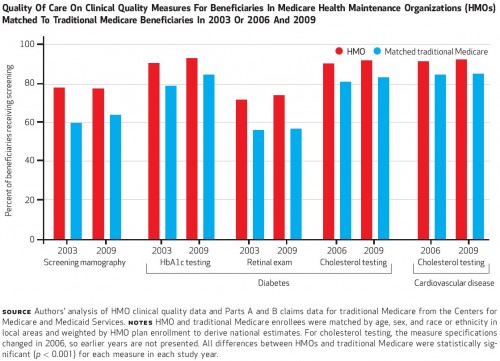
Comparing a large cohort (at least 100,000, though varying by measure) of MA HMO enrollees matched to FFS beneficiaries in the same areas over 2003-2009, and controlling for demographics and health status, the investigators found that the MA plans provided statistically significantly higher quality. The chart below provides some results for selected years and measures. With the exception of beneficiary ratings of doctors, results for other measures are similar.
 The researchers report:
The researchers report:
Our study comparing quality of care in Medicare HMOs and traditional Medicare produced three main findings. First, performance measures of breast cancer screening, diabetes care, and cholesterol testing for cardiovascular disease during 2003–09 were consistently better in HMOs than in traditional Medicare overall, but differences in breast cancer screening and HbA1c testing narrowed somewhat as traditional Medicare improved. Second, rates of influenza and pneumococcal vaccinations in 2003 were higher in HMOs than in traditional Medicare but were much more similar by 2009. Third, ratings of personal physicians were less favorable for HMOs relative to traditional Medicare in 2003, but by 2009 they were better in HMOs than in traditional Medicare. Given very similar rates of outpatient visits in Medicare HMOs and traditional Medicare in 2009, our results suggest that the effects on the quality of ambulatory care provided by more integrated delivery systems in Medicare HMOs may have outweighed the potential incentives to restrict care under capitated payments.These results bear on recent policy developments, as discussed by the authors. First, the Affordable Care Act (ACA) includes quality bonus payments to MA plans that didn't exist during the period of focus of this study. These bonuses should only increase incentives for quality, though their effect remains to be seen. Second, accountable care organizations (ACOs) are also promoted by the law and provide incentives for Medicare providers to improve quality. This study provides some encouragement that organizations may be able to do so, as does the recent news about Pioneer ACOs. Finally, other recent work suggests that the patterns of practice encouraged by MA plans spills over into other parts of the health system. Though that study did not examine the quality measures discussed above or the same ones in my prior post, it is at least suggestive that higher MA quality might also cause higher quality more generally. Even if all of the above is true -- and one should always be cautious about drawing conclusions from a small number of studies -- it is still relevant to ask whether the cost of MA plans is worth the benefits they may offer. They are still paid more than the cost of FFS Medicare. How much would quality suffer if they were not?