
The COVID-19 pandemic has magnified the need to address long-standing health disparities and the role of social determinants of health (SDOH) in addressing health equity. Still, evaluating social determinant interventions in terms of health care costs is not enough—addressing equity challenges requires an interest or involvement beyond a medical intervention that includes a social services component.
As part of a webinar series from AcademyHealth and the National Pharmaceutical Council (NPC) on key issues in health and spending, Garth Graham from Google/YouTube moderated a discussion called “Understanding the Costs and True Benefits of SDOH Investments,” that also included Robert Dubois of NPC, Evelyn Gallego from the Gravity Project, and Andrew Renda, from Humana’s Bold Goal initiative.
Evaluating and Addressing Social Risk
While the discussion underscored the necessity of health spending to address social risk factors, the speakers brought to light other indicators when determining whether SDOH-related interventions and expenditures lead to health improvements and reduce costs. For example, access to a quality education is a powerful indicator for SDOH, and given the broad impact on education due to the COVID-19 pandemic, this issue will be an ongoing challenge for years to come. Other factors like quality housing, transportation, and food security also were noted and should be incorporated into clinical encounters and other interventions.
According to Evelyn Gallego’s Gravity Project, which recommends standards for social risk factor data, “growing evidence demonstrates strong links between social risk and an individual's health and health care utilization.” During the panel, Gallego noted the value of determining these social risks beyond having a patient complete a screening form at a physician’s office, but instead collecting data to engage the individual in a direct, close-looped intervention. She provided the example of referring someone to a foodbank. Such interventions are valuable, Andrew Renda highlighted, because if a patient is food insecure, they will be likely to spend their money on food over health care, risking worsening chronic conditions. Another example beyond clinical interventions, according to Gallego, was providing a ride to a high-risk patient to their medical appointment. This is a low-cost social intervention that could reduce high-cost medical interventions.
Challenges with Evaluating the Impact and Return on Investment (ROI)
In order to determine whether an intervention reduced costs and provided non-health care benefits, health professionals must be intentional when conducting SDOH-related studies and provide the same rigor that would be given to a clinical study. Studies related to SDOH are often incomplete and few include outcomes measurements or an assessment of patient quality-of-life to understand if there was improvement, according to Robert Dubois. He noted that the poor quality of the studies suggests that there isn’t enough information to determine which interventions work, or how to design an effective one, what makes it successful, and how to optimize ROI to develop best practices.
Dubois highlighted the importance of knowing if an intervention led to health improvements before investing in that intervention. In order to develop best practices for interventions, more rigorous data collection and measurement is needed to determine what works and allows other to replicate success.
Gallego also discussed an issue she encountered when assessing the success of an intervention: the lack of standard codes to represent the data, which meant everyone was documenting information differently. Without consistency, there was no way to measure whether the clinical and community-based interventions led to the right outcomes.
Utilizing and Standardizing SDOH Data
Gallego highlighted that defining concepts related to interventions is key to measuring successful outcomes . There must be agreement on how to collect data, including defining the terms and then coding those terms to represent information because each system does it differently. Measuring the success of social determinant interventions requires data interoperability to allow for the seamless exchange of information regardless of the data source—whether it is an electronic health record (EHR) or community-based organization platform. Success is creating a way to exchange data across platforms regardless of the source and engaging the individual patient and consumer. A standardized data infrastructure is needed to rapidly measure, capture, and represent data accurately.
Similarly, Renda highlighted that no SDOH data ecosystem currently exists as there is for clinical data. In collaboration with partners, his organization developed a methodology to standardize SDOH data (see image below), starting with the need to categorize SDOH data to screen participants before the data enters a data governance process to become standardized.
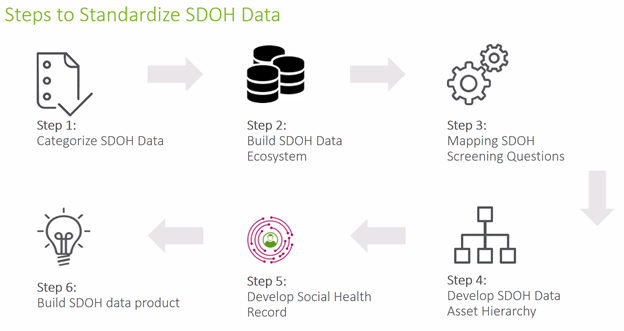
Humana, Renda noted, also is working to move beyond data that is primarily clinical to include information about social risk data to better understand patient needs. This data system is needed to build the right data product, and track screenings, outcomes, and other insights to focus on which social needs to prioritize.
In closing, the panel agreed that the lack of data collection and infrastructure provides an opportunity to shape how we collect data to understand ROI of interventions, but that data standardization and measurable improvements in patient outcomes are key to scaling future SDOH interventions. And, an understanding of the intervention costs, savings, and time horizon for a return on the investments is equally important.