In the United States, the burden of medical debt on patients has reached an alarming $195 billion, with 1 in 10 Americans owing more than $250 in medical bills. Notably, these burdens are not distributed evenly. A larger portion of Black adults (16 percent) report grappling with medical debt compared to their White counterparts (9 percent). Adults with lower incomes are more likely to have medical debt (12 percent) than adults with higher incomes (4 percent). But economic impacts can be so much more than medical bills alone, as conversations with our recent project participants clearly highlight:
“The impact of a serious illness is personal first - management of family, job, psycho-social - and then it is medical” (key informant)
“It all comes from one wallet” (Roundtable participant)
Economic impacts on patients can be significant and wide ranging, leading to poorer health outcomes and lost productivity that effect society as a whole.
Researchers and decisionmakers increasingly recognize the importance of considering this broader range of economic impacts on patients and caregivers at different stages of the patient journey. However, research plans and data infrastructure have not evolved in step. Often, research is confined to readily available data rather than measuring what is most costly from the patient perspective--things like missed time with family, lost work, lost education, etc. This can lead to little progress in defining concrete actions to improve research measures to support/characterize real-world implications for patients.
Innovation and Value Initiative (IVI) and AcademyHealth partnered, through a project supported by a Eugene Washington PCORI Engagement Award, to convene a participatory process and develop a framework for researchers that captures the full range of economic impacts on patients and caregivers. The project included two parts: (1) conducting an environmental scan to identify existing methods for defining economic impacts in health-related research; and (2) iterative stakeholder engagement to develop a draft framework (Fig 1).
Figure 1. Stakeholder engagement activities conducted by the IVI-AcademyHealth project with funding from PCORI.
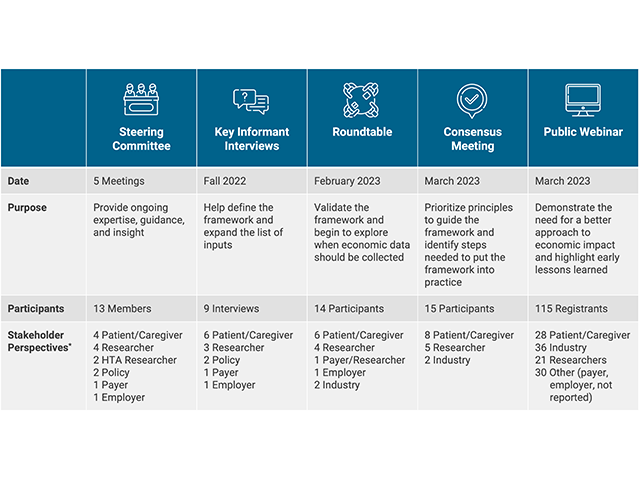
During each activity, a diverse array of patients, caregivers and other stakeholders (including the authors here) contributed their experience working with economic impacts, recommendations for development and refinement of the framework, and potential future applications of the framework. The organizing framework that emerged from these discussions (Fig 2) highlights the wide range of the often-overlooked economic impacts that patients and caregivers face daily, by placing patients and caregivers at the center of the picture. This work was presented in a poster at the 2023 PCORI Annual Meeting on October 5.
Discussions with stakeholders throughout the project emphasized the need to frame economic impacts through an equity lens, taking into account the life journey. This recognizes that the lived experience of economic impacts will be different for different people, they may change over time, they may interact with each other and other factors (intersectionality), and they may ultimately become drivers of new health outcomes.
Figure 2. Interactive framework to understand economic impacts on patients and caregivers.
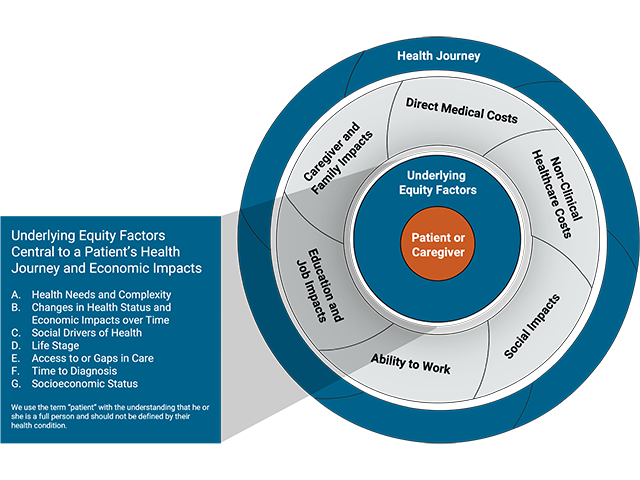
These are then surrounded by the six domains of economic impacts. The domains may also overlap or intersect, reflecting the many ways that patients and caregivers experience economic burdens in the context of their lives.
- Direct Medical Costs: costs of care paid to a healthcare provider or healthcare system.
- Non-Clinical Healthcare Costs: direct costs of care that are not paid into the healthcare system.
- Social Impacts: impacts such as time spent negotiating with insurance companies or accessing social services.
- Ability to Work: costs related to productivity, sick days, days off from work, etc.
- Education and Job Attainment: impacts such as career choice or educational achievement.
- Caregiver and Family Impacts: all types of economic impacts that caregivers experience because of the primary patient’s illness or health condition.
Finally, this is all enclosed within the individual’s health journey over time. The context of the specific condition, or set of conditions, will ultimately frame the way these economic and equity factors come together and interact in a given person at a given point in time.
This framework offers a powerful new tool for researchers to comprehensively co-create with patients a more holistic approach to understanding the patient and caregiver experience. Applying the framework can enhance how we generate evidence to better meet the needs of patients, providers, and policymakers. It can start to build the foundation for a robust data ecosystem, addressing gaps in measuring social impacts and education or job attainment so that these broader factors can be incorporated into effectiveness research and health technology assessment. Specifically, this tool can be used to guide discussions with stakeholders about important determinants and outcomes of care, inform protocols for data collection, drive the development of new data infrastructure, guide the specification of statistical models, and aid in the interpretation of findings—all in service of a more complete and comprehensive understanding of the factors most important to patients and their caregivers.
Applying this framework requires careful attention to how researchers operationalize it and the availability of mechanisms to hold the field accountable to its message. We encourage researchers, funders, and other stakeholders to adopt this framework and take these actions:
- Expand Data Collection: Cultivate multi-stakeholder partnerships to measure a broader range of economic impacts.
- Drive culture change: Orient researchers and decision-makers to patient-centered economic outcomes that are outside of traditional measures in health care data.
- Engage patients: Harness the expertise of underserved and underrepresented communities in leadership roles to identify priorities and solutions.
Recognizing and examining broad health care economic impacts on patients and caregivers is critical to addressing health disparities and creating value for patients and systems.